Pneumonia Patch In Chest
Management of spontaneous pneumothorax British Thoracic Society pleural disease guideline 2. Slovenska Televizia 2 Program. Introduction. The term pneumothorax was first coined by Itard and then Laennec in 1. At that time, most cases of pneumothorax were secondary to tuberculosis, although some were recognised as occurring in otherwise healthy patients pneumothorax simple. This classification has endured subsequently, with the first modern description of pneumothorax occurring in healthy people primary spontaneous pneumothorax, PSP being that of Kjrgaard. It is a significant global health problem, with a reported incidence of 1. Secondary pneumothorax SSP is associated with underlying lung disease, in distinction to PSP, although tuberculosis is no longer the commonest underlying lung disease in the developed world. The consequences of a pneumothorax in patients with pre existing lung disease are significantly greater, and the management is potentially more difficult. Combined hospital admission rates for PSP and SSP in the UK have been reported as 1. With regard to the aetiology of pneumothorax, anatomical abnormalities have been demonstrated, even in the absence of overt underlying lung disease. Subpleural blebs and bullae are found at the lung apices at thoracoscopy and on CT scanning in up to 9. PSP,5. 6 and are thought to play a role. More recent autofluorescence studies. Small airways obstruction, mediated by an influx of inflammatory cells, often characterises pneumothorax and may become manifest in the smaller airways at an earlier stage with emphysema like changes ELCs. C# Create Text File And Write To It'>C# Create Text File And Write To It. A newly released image shows comedian Kevin Hart resting his head on a womans chest and clutching her thigh in a steamy video at the centre of an FBI extortion probe. Management of spontaneous pneumothorax British Thoracic Society pleural disease guideline 2010. Procalcitonin PCT is a peptide precursor of the hormone calcitonin, the latter being involved with calcium homeostasis. It was first identified by Leonard J. Deftos. Hepatitis A, B, and C are viral infections that together affect an estimated 5 to 6 of Americans. Get indepth hepatitis information here about hepatitis symptoms. Smoking has been implicated in this aetiological pathway, the smoking habit being associated with a 1. Patients with PSP tend to be taller than control patients. The gradient of negative pleural pressure increases from the lung base to the apex, so that alveoli at the lung apex in tall individuals are subject to significantly greater distending pressure than those at the base of the lung, and the vectors in theory predispose to the development of apical subpleural blebs. Although it is to some extent counterintuitive, there is no evidence that a relationship exists between the onset of pneumothorax and physical activity, the onset being as likely to occur during sedentary activity. Despite the apparent relationship between smoking and pneumothorax, 8. PSP. 1. 4 The risk of recurrence of PSP is as high as 5. Risk factors for recurrence of SSP include age, pulmonary fibrosis and emphysema. Thus, efforts should be directed at smoking cessation after the development of a pneumothorax. The initial British Thoracic Society BTS guidelines for the treatment of pneumothoraces were published in 1. Pneumonia Patch In Chest' title='Pneumonia Patch In Chest' />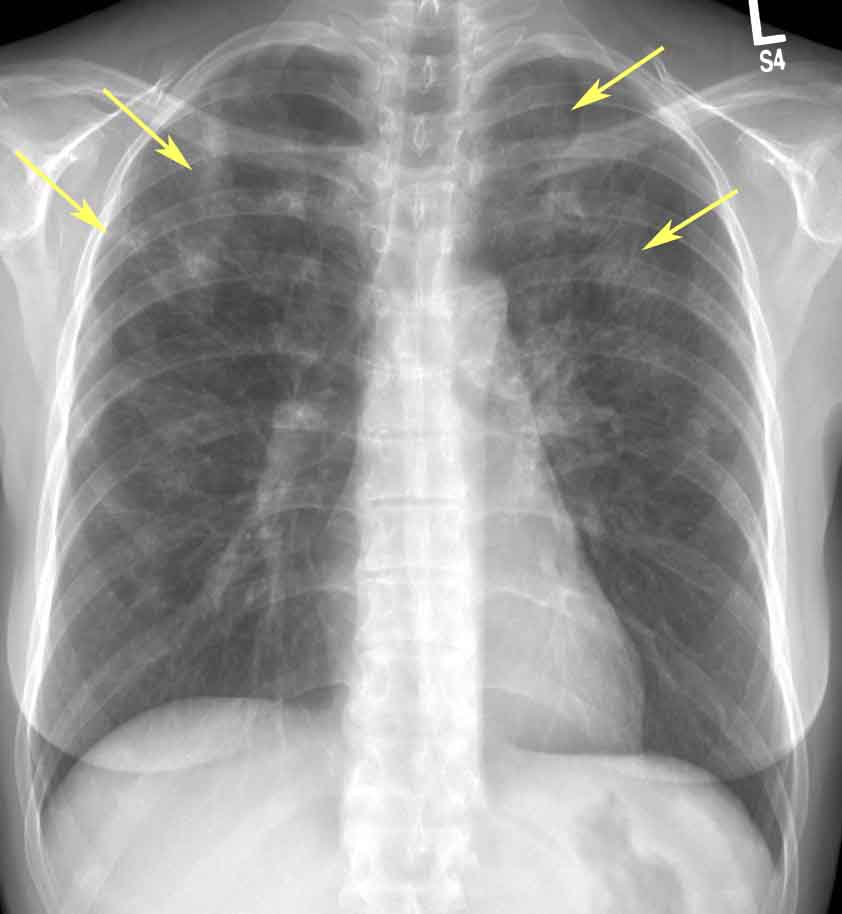 Later studies suggested that compliance with these guidelines was improving but remained suboptimal at only 2. A E staff. Clinical guidelines have been shown to improve clinical practice,1. The second version of the BTS guidelines was published in 2. It included algorithms for the management of PSP and SSP but excluded the management of trauma. This guideline seeks to consolidate and update the pneumothorax guidelines in the light of subsequent research and using the SIGN methodology. Traumatic pneumothorax is not covered by this guideline. SSP is associated with a higher morbidity and mortality than PSP. DStrong emphasis should be placed on smoking cessation to minimise the risk of recurrence. DPneumothorax is not usually associated with physical exertion. DClinical evaluation. Symptoms in PSP may be minimal or absent. In contrast, symptoms are greater in SSP, even if the pneumothorax is relatively small in size. DThe presence of breathlessness influences the management strategy. DSevere symptoms and signs of respiratory distress suggest the presence of tension pneumothorax. DThe typical symptoms of chest pain and dyspnoea may be relatively minor or even absent,2. Many patients especially those with PSP therefore present several days after the onset of symptoms. The longer this period of time, the greater is the risk of re expansion pulmonary oedema RPO. In general, the clinical symptoms associated with SSP are more severe than those associated with PSP, and most patients with SSP experience breathlessness that is out of proportion to the size of the pneumothorax. These clinical manifestations are therefore unreliable indicators of the size of the pneumothorax. When severe symptoms are accompanied by signs of cardiorespiratory distress, tension pneumothorax must be considered. The physical signs of a pneumothorax can be subtle but, characteristically, include reduced lung expansion, hyper resonance and diminished breath sounds on the side of the pneumothorax. Added sounds such as clicking can occasionally be audible at the cardiac apex. The presence of observable breathlessness has influenced subsequent management in previous guidelines. In association with these signs, cyanosis, sweating, severe tachypnoea, tachycardia and hypotension may indicate the presence of tension pneumothorax see later section. Arterial blood gas measurements are frequently abnormal in patients with pneumothorax, with the arterial oxygen tension Pao. Pa in 7. 5 of patients,3. The hypoxaemia is greater in cases of SSP,3. Pao. 2 being lt 7. Pa, together with a degree of carbon dioxide retention in 1. Pulmonary function tests are poor predictors of the presence or size of a pneumothorax. The diagnosis of pneumothorax is usually confirmed by imaging techniques see below which may also yield information about the size of the pneumothorax, but clinical evaluation should probably be the main determinant of the management strategy as well as assisting the initial diagnosis. Imaging. Initial diagnosis. Standard erect chest x rays in inspiration are recommended for the initial diagnosis of pneumothorax, rather than expiratory films. AThe widespread adoption of digital imaging PACS requires diagnostic caution and further studies since the presence of a small pneumothorax may not be immediately apparent. DCT scanning is recommended for uncertain or complex cases. DThe following numerous imaging modalities have been employed for the diagnosis and management of pneumothorax Standard erect PA chest x ray. Lateral x rays. Expiratory films. Supine and lateral decubitus x rays. Ultrasound scanning. Digital imaging. CT scanning. Standard erect PA chest x ray. This has been the mainstay of clinical management of primary and secondary pneumothorax for many years, although it is acknowledged to have limitations such as the difficulty in accurately quantifying pneumothorax size. Major technological advances in the last decade have resulted in the advent of digital chest imaging, so that conventional chest films are no longer easily available in clinical practice in the UK or in many other modern healthcare systems. The diagnostic characteristic is displacement of the pleural line. In up to 5. 0 of cases an air fluid level is visible in the costophrenic angle, and this is occasionally the only apparent abnormality. The presence of bullous lung disease can lead to the erroneous diagnosis of pneumothorax, with unfortunate consequences for the patient. If uncertainty exists, then CT scanning is highly desirable see below. Lateral x rays. These may provide additional information when a suspected pneumothorax is not confirmed by a PA chest film. Expiratory films. These are not thought to confer additional benefit in the routine assessment of pneumothorax.
Later studies suggested that compliance with these guidelines was improving but remained suboptimal at only 2. A E staff. Clinical guidelines have been shown to improve clinical practice,1. The second version of the BTS guidelines was published in 2. It included algorithms for the management of PSP and SSP but excluded the management of trauma. This guideline seeks to consolidate and update the pneumothorax guidelines in the light of subsequent research and using the SIGN methodology. Traumatic pneumothorax is not covered by this guideline. SSP is associated with a higher morbidity and mortality than PSP. DStrong emphasis should be placed on smoking cessation to minimise the risk of recurrence. DPneumothorax is not usually associated with physical exertion. DClinical evaluation. Symptoms in PSP may be minimal or absent. In contrast, symptoms are greater in SSP, even if the pneumothorax is relatively small in size. DThe presence of breathlessness influences the management strategy. DSevere symptoms and signs of respiratory distress suggest the presence of tension pneumothorax. DThe typical symptoms of chest pain and dyspnoea may be relatively minor or even absent,2. Many patients especially those with PSP therefore present several days after the onset of symptoms. The longer this period of time, the greater is the risk of re expansion pulmonary oedema RPO. In general, the clinical symptoms associated with SSP are more severe than those associated with PSP, and most patients with SSP experience breathlessness that is out of proportion to the size of the pneumothorax. These clinical manifestations are therefore unreliable indicators of the size of the pneumothorax. When severe symptoms are accompanied by signs of cardiorespiratory distress, tension pneumothorax must be considered. The physical signs of a pneumothorax can be subtle but, characteristically, include reduced lung expansion, hyper resonance and diminished breath sounds on the side of the pneumothorax. Added sounds such as clicking can occasionally be audible at the cardiac apex. The presence of observable breathlessness has influenced subsequent management in previous guidelines. In association with these signs, cyanosis, sweating, severe tachypnoea, tachycardia and hypotension may indicate the presence of tension pneumothorax see later section. Arterial blood gas measurements are frequently abnormal in patients with pneumothorax, with the arterial oxygen tension Pao. Pa in 7. 5 of patients,3. The hypoxaemia is greater in cases of SSP,3. Pao. 2 being lt 7. Pa, together with a degree of carbon dioxide retention in 1. Pulmonary function tests are poor predictors of the presence or size of a pneumothorax. The diagnosis of pneumothorax is usually confirmed by imaging techniques see below which may also yield information about the size of the pneumothorax, but clinical evaluation should probably be the main determinant of the management strategy as well as assisting the initial diagnosis. Imaging. Initial diagnosis. Standard erect chest x rays in inspiration are recommended for the initial diagnosis of pneumothorax, rather than expiratory films. AThe widespread adoption of digital imaging PACS requires diagnostic caution and further studies since the presence of a small pneumothorax may not be immediately apparent. DCT scanning is recommended for uncertain or complex cases. DThe following numerous imaging modalities have been employed for the diagnosis and management of pneumothorax Standard erect PA chest x ray. Lateral x rays. Expiratory films. Supine and lateral decubitus x rays. Ultrasound scanning. Digital imaging. CT scanning. Standard erect PA chest x ray. This has been the mainstay of clinical management of primary and secondary pneumothorax for many years, although it is acknowledged to have limitations such as the difficulty in accurately quantifying pneumothorax size. Major technological advances in the last decade have resulted in the advent of digital chest imaging, so that conventional chest films are no longer easily available in clinical practice in the UK or in many other modern healthcare systems. The diagnostic characteristic is displacement of the pleural line. In up to 5. 0 of cases an air fluid level is visible in the costophrenic angle, and this is occasionally the only apparent abnormality. The presence of bullous lung disease can lead to the erroneous diagnosis of pneumothorax, with unfortunate consequences for the patient. If uncertainty exists, then CT scanning is highly desirable see below. Lateral x rays. These may provide additional information when a suspected pneumothorax is not confirmed by a PA chest film. Expiratory films. These are not thought to confer additional benefit in the routine assessment of pneumothorax.



